Promo Codes

-

Nigel Farage Claims He Has ‘Never Directly Experienced Racial Abuse’ – Mirror Brief
-
Test Your Knowledge of Iconic Lines from Timeless Sci-Fi Novels – Mirror Brief
-
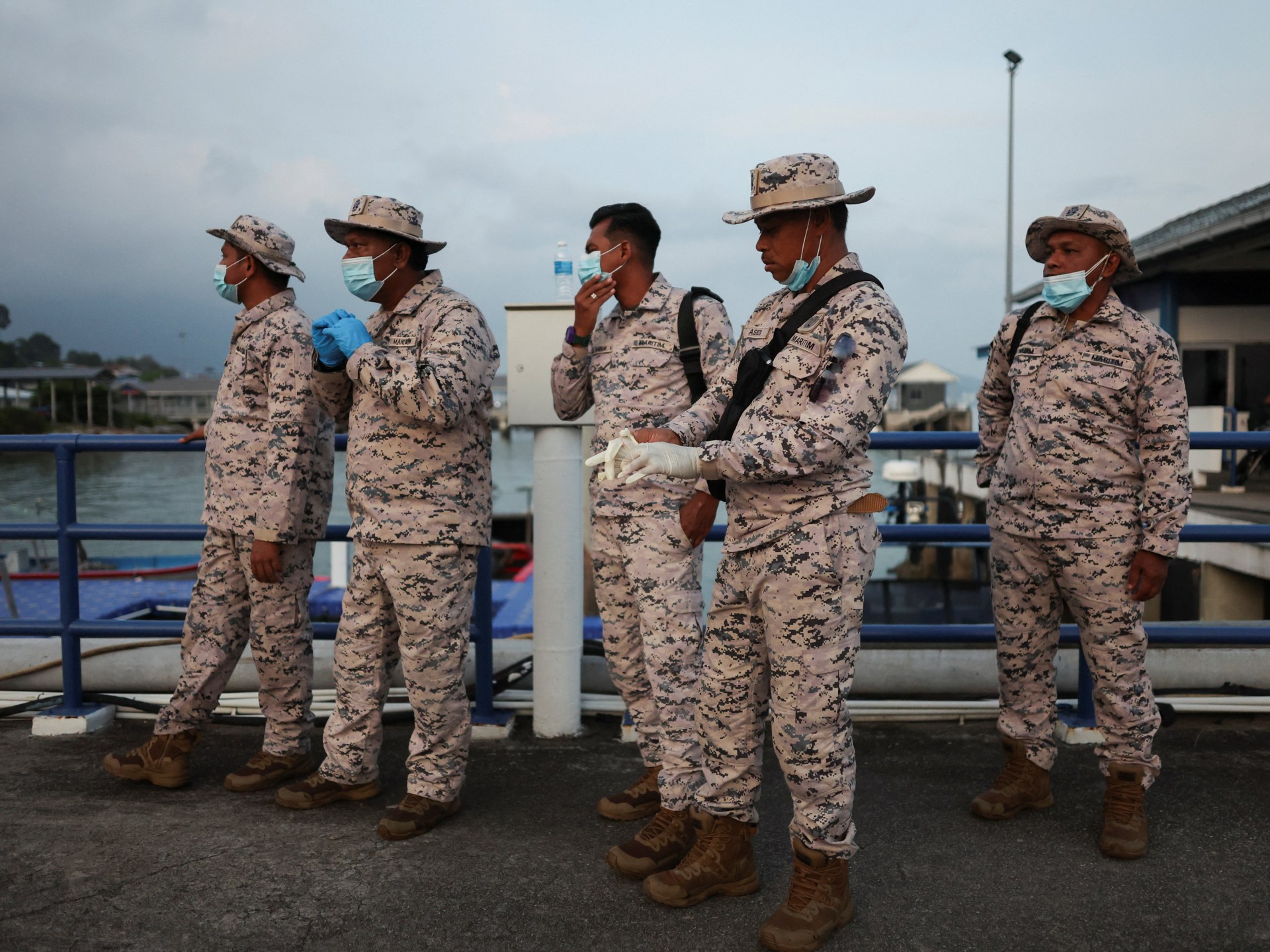
Trump Administration Terminates Temporary Immigration Status for Citizens of Myanmar – Mirror Brief
-

Dsquared2’s Menswear Collection for Pre-Fall 2026 – Mirror Brief
-

Suggest Your Favorite Outdoor Winter Activities in the UK – Mirror Brief
-

US Urges Europe to Address Taxation of Major Tech Firms – Mirror Brief
-

Leaked BBC Memo Author Asserts Broadcaster Lacks Institutional Bias – Latest Developments – Mirror Brief
-

Jill Freud, Beloved Actress from Love Actually and Muse for Narnia’s Lucy, Passes Away at 98 – Mirror Brief
-
The Impact of OpenAI’s Modifications on User Reactions – Mirror Brief
-

Argentina Files Complaint and Calls for Investigation into Tom Curry Over Alleged Tunnel Altercation – Mirror Brief
-

UN Climate Discussions Fall Short of New Commitments on Fossil Fuels – Mirror Brief
-

Princess of Wales Advocates for Breaking the Stigma Surrounding Addiction – Mirror Brief
-

Ukrainians Respond to Proposal for Concluding Russia’s Conflict – Mirror Brief
-

David Cameron Discloses His Battle with Prostate Cancer – Mirror Brief
-

Nine Distinctive Airbnb Experiences to Enjoy on Your Upcoming London Getaway – Mirror Brief
-

PwC Executive Warns AI Poses Risk to Graduate Positions – Mirror Brief
-
Customer Dilemma
-

Exploring the Surge of a £1 Million Glastonbury Ticket Fraudster – Mirror Brief
-
7,117 Puzzles to Solve – Mirror Brief
-
Are Brain-Decoding Devices a Threat to Individual Privacy? – Mirror Brief
-

Rogers’ Unique Yet Intriguing Free-Kick Method – Mirror Brief
-

Reeves Set to Tackle Benefit Fraud While Removing Two-Child Limit in Budget 2025 – Mirror Brief
-

Rubio Celebrates Significant Advancements in Ukraine Peace Negotiations – Mirror Brief
-

Think Tank Advocates for Smaller Hospitals to Address NHS ‘Permacrisis’ – Mirror Brief
-

Exciting Pre-Launch Deals on Apple TV+, MasterClass, Fubo, Rosetta Stone, and More – Mirror Brief
-

The Influence of ‘Mutiny on the Bounty’ on the Oscars’ Supporting Actor Category – Mirror Brief
-

Zia Yusuf of Reform UK Labels Nathan Gill as ‘Outdated History’ – Mirror Brief
-

Ending the Sacrifice of Millions for Human Health – Mirror Brief
-

The Significance of John Williams’ Insights – Mirror Brief
-

A Coastal Maine Town Becomes a Festive Wonderland Each December Featuring a Lobster Trap Christmas Tree – Mirror Brief